Pregnancy puts new demands on a woman’s body. It can alter
the course of some medical conditions a woman may have before pregnancy, and
some conditions can affect the course of pregnancy. A woman with such a medical
condition can have a healthy baby. An extra effort will be required, however,
so that the woman’s general health and her pregnancy can be followed more
closely.
If you have a condition that could complicate your
pregnancy, your doctor may order additional tests and ask you to make extra
prenatal visits or attend special clinics. You may need to stay in the hospital
or to monitor your condition yourself at home. Your doctor may work with a team
of experts to provide any special care you may need.
High Blood Pressure
Hypertension, or high blood pressure, occurs when the
pressure of the blood in the arteries reaches levels that are greater than
normal. This condition can be preexisting (before pregnancy) and chronic
(long-term), or it can arise during pregnancy. High blood pressure that arises
during pregnancy can be a sign of a condition called preeclampsia (also known
as toxemia). These two conditions – chronic high blood pressure and
preeclampsia affect pregnancy and its outcome in different ways. Depending on
how severe these conditions are, both the mother and fetus can be affected.
The heart pumps blood rich in oxygen through the arteries
(light blood vessels) to all parts of the body. Blood returns to the heart
through the veins (dark blood vessels).If a blood pressure reading is 110/80,
110 is the pressure in the arteries when the heart is contracting, or the
systolic pressure. The lower number, 80, is the pressure in the arteries when
the heart is relaxed, or the diastolic pressure.
Measuring Blood
Pressure
Blood pressure is checked with a stethoscope and an
instrument made of an inflatable cuff and a pressure gauge (sphygmomanometer).
A blood pressure reading is made up of two numbers separated by a slash, for
example, 110/80. (You may hear this referred to as”110 over 80”). The first
number is the pressure in the arteries when the heart contracts. This is called
the systolic pressure. The second number is the pressure in the arteries when
the heart is relaxed between contractions. This is the diastolic pressure.
Blood pressure changes often during the day. It can rise if
you are excited or if you exercise. It usually falls when you are resting.
These temporary changes in blood pressure that occur in response to some
activity or event are normal. It is only when a person’s blood pressure stays
high for some time that it requires attention.
Because of the normal ups and downs in blood pressure, if
your doctor finds one high reading, he or she will want to see whether it is
your normal level by taking another reading. Your normal blood pressure can be
an average of several readings taken at rest.
Blood pressure varies from person to person, so everyone’s
blood pressure is different. In nonpregnant adults, readings less that 130/80
are usually normal, and become abnormal when pressures reach above 140/90.
Some blood pressure levels that may see normal could be too
high in a pregnant woman. For instance, a reading of 120/85 would be considered
too high for a pregnant woman whose normal reading was 90/70. As a rule, any
increase of 30 or more in the systolic reading or 15 or more in the diastolic
reading can be a sign of high blood pressure in pregnancy.
It is normal for blood pressure to drop slightly during the
middle part of pregnancy and then return to pregnancy levels during the latter
part of pregnancy. Because of these changes, it is important to have your blood
pressure measured before pregnancy or in early pregnancy so your doctor will
know what is normal for you. As a part of prenatal care, a woman’s blood
pressure is checked at each visit.
Chronic High Blood Pressure
High blood pressure can be present when a woman becomes
pregnant. Diet, life style, and heredity con tribute to chronic high blood
pressure. Over the course of her life, a woman with untreated high blood
pressure is more likely to have a heart attack or stroke. She is also at higher
risk for having problems during pregnancy. These include having a baby that is
too small or separation of the placenta from the wall of the uterus before the
fetus is born.
Before you get pregnant chronic hypertension should be
brought under control with diet, weight loss, and possibly medication. During
pregnancy, regular checkups are important to detect any changes in your
condition that may signal a problem.
What is Preeclampsia?
High blood pressure that occurs for the first time in the
second half of pregnancy along with protein in the urine and, usually, fluid
retention is called preeclampsia. It affects about 7 out of every 100 women who
become pregnant. It is not known what causes preeclampsia, although women who
have chronic high blood pressure are more likely to develop it. Most women with
preeclampsia, however, have never had high blood pressure before. Preeclampsia
usually occurs with first pregnancies and often does not recur in later
pregnancies except in women who have chronic hypertension or other diseases
affecting the blood vessels. With preeclampsia, blood pressure returns to
normal levels after pregnancy, whereas chronic hypertension remains after
delivery.
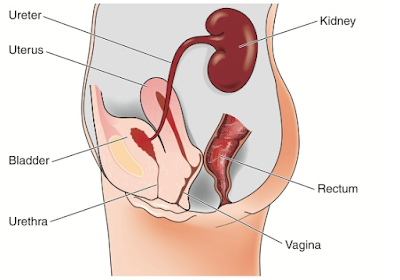
The blood vessels in the uterus supply blood to the
placenta, through which the fetus is nourished and given oxygen. When a woman
has preeclampsia, the blood flow through these vessels is reduced. The severity
of the condition and the time in pregnancy when it occurs determines the degree
of risk to the fetus.
When blood pressure increases during pregnancy, your doctor
may recommend bed rest. Frequently, the blood pressure will improve or return
to normal with rest. When resting the woman may be advised to lie on her
side-this position improves the flow of blood to the uterus and kidneys. Some
doctors hospitalize women as soon as there is a slight increase in blood
pressure; others wait until there is evidence that bed rest at home has not
helped to reduce blood pressure.
Caption:Bed rest may be prescribed for a woman with
preeclampsia.
Preeclampsia occurs in degrees, from mild to severe, and can
gradually worsen or improve. If preeclampsia is detected in mild stages and
controlled by bed rest and medication, the effects on the baby can be reduced.
The goal, all other factors permitting, is to allow the pregnancy to continue
until the fetus is old enough to be born.
When preeclampsia occurs early and is severe, early delivery
may be necessary. A premature body is underweight and may have trouble
breathing because the lungs are not fully developed. When preeclampsia is
associated with chronic hypertension, the placenta can separate from the uterus
and result in stillbirth. Preeclampsia can also be linked to poor fetal growth.
Severe preeclampsia can also be linked to poor fetal growth. Severe
preeclampsia affects almost all of the mother’s organs, such as the blood
system, liver, kidneys, and brain. Convulsions can occur without warning with preeclampsia.
When this occurs, the disease is called eclampsia. The treatment for very
severe preeclampsia or eclampsia is to deliver the fetus, either by inducing
labor or performing a cesarean birth.